Types of Orthotics for Plantar Fasciitis
If you have plantar fasciitis, an inflammation of the ligament that runs along the bottom of the foot, then you likely deal with foot and heel pain. One way to relieve plantar fasciitis symptoms is to wear orthotics. There are several different types of orthotics used to treat plantar fasciitis. Heel cups or pads are placed in the back of your shoes. They lift up the heel slightly and cushion it, relieving tension in the Achilles tendon and plantar fascia. Shoe insoles are inserted into the shoes and run along the entire sole of the foot. They support the foot arches to reduce strain on the plantar fascia ligament. Night splints are devices that hold the foot in place while you sleep, gently stretching your ligaments and tendons to avoid heel pain in the morning. To find out if orthotics are right for you, please consult with a podiatrist.
If you are having discomfort in your feet and would like to try orthotics, contact one of our podiatrists from Coastal Foot & Ankle Wellness Center, LLC. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact one of our offices located in St. Augustine, and Palatka, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot Orthotics
Orthotics are shoe inserts that are meant to correct an irregular walking gait or provide cushioning to the feet. Orthotics come in a variety of different models and sizes, including over-the-counter and customizable variants. Customizable orthotics can be shaped and contoured to fit inside a specific shoe and are typically prescribed through a podiatrist who specializes in customized footwear and orthotics design and management.
Orthotics are beneficial because they can help prevent injuries from occurring and provide cushioning to keep pain levels down to a minimum. They also allow for the correct positioning of the feet. Orthotics can act as shock absorbers to help remove pressure from the foot and ankle. Therefore, orthotics can make bodily movements, such as walking and running, become more comfortable as well as help prevent the development of certain foot conditions.
Orthotics alleviate pain and make the foot more comfortable by slightly altering the angle at which the foot strikes the ground surface, therefore controlling the movement of the foot and ankle. Orthotics come in different variants and can be made of various materials. To determine what type of orthotic is most suited to your feet and your needs, it is best to consult your podiatrist. He or she will be able to recommend a type of orthotic that can help improve your foot function or prescribe a custom orthotic to best fit your feet.
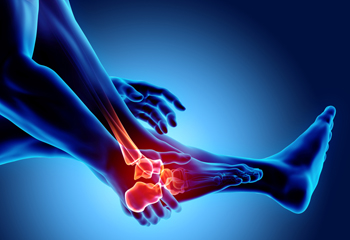
Causes of Pain on the Outside of the Foot
If you are feeling pain along the outside of your foot, it is important to consider the exact location, onset, and type of pain that you are facing, as well as any co-occurring symptoms. Pain along the outside of the ankle that is accompanied by swelling, bruising, and ankle instability may be indicative of an ankle sprain. Pain along the outside of the foot that is at its worst in the morning or when running or walking on uneven ground may be cuboid syndrome. Pain on the outside of the big toe joint, especially when accompanied by toe deformity and redness, is usually indicative of a bunion. Other common causes of pain on the outside of the foot include peroneal tendonitis, stress fractures, corns and calluses, and posterior tibial tendonitis. If you are experiencing pain on the outside of your foot, please consult with a podiatrist.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with one of our podiatrists from Coastal Foot & Ankle Wellness Center, LLC. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact one of our offices located in St. Augustine, and Palatka, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
Our feet are arguably the most important parts of our bodies because they are responsible for getting us from place to place. However, we often don’t think about our feet until they begin to hurt. If you have pain in your feet, you need to first determine where on the foot you are experiencing it to get to the root of the problem. The most common areas to feel pain on the foot are the heel and the ankle.
Heel pain is most commonly attributed to a condition called plantar fasciitis. Plantar fasciitis occurs when the plantar fascia, which is the band of tough tissue connecting the heel bone to the toes becomes inflamed. Plantar fasciitis pain is usually worse in the morning, and it tends to go away throughout the day. If you have plantar fasciitis, you should rest your foot and do heel and foot muscles stretches. Wearing shoes with proper arch support and a cushioned sole has also been proven to be beneficial.
Some common symptoms of foot pain are redness, swelling, and stiffness. Foot pain can be dull or sharp depending on its underlying cause. Toe pain can also occur, and it is usually caused by gout, bunions, hammertoes, ingrown toenails, sprains, fractures, and corns.
If you have severe pain in your feet, you should immediately seek assistance from your podiatrist for treatment. Depending on the cause of your pain, your podiatrist may give you a variety of treatment options.
Rheumatoid Arthritis Statistics
Rheumatoid arthritis (RA) is an autoimmune disease in which the body’s immune system attacks its own, otherwise healthy cells. The cells that are frequently attacked are those of the synovium, the soft tissue that lines the joints. The small joints of the feet and ankles are often affected, leading to symptoms such as foot and ankle pain, joint swelling, stiffness, and reduced mobility. RA affects millions of adults annually. In 2020, approximately 53 of every 100,000 women and 29 of every 100,000 men had RA. Women are more likely than men to develop RA at an early age. If you have RA and are experiencing foot and ankle pain, a podiatrist can help you relieve symptoms and maintain your foot health and mobility.
Because RA affects more than just your joints, including the joints in your feet and ankles, it is important to seek early diagnosis from your podiatrist if you feel like the pain in your feet might be caused by RA. For more information, contact one of our podiatrists of Coastal Foot & Ankle Wellness Center, LLC. Our doctors will assist you with all of your podiatric concerns.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disorder in which the body’s own immune system attacks the membranes surrounding the joints. Inflammation of the lining and eventually the destruction of the joint’s cartilage and bone occur, causing severe pain and immobility.
Rheumatoid Arthritis of the Feet
Although RA usually attacks multiple bones and joints throughout the entire body, almost 90 percent of cases result in pain in the foot or ankle area.
Symptoms
- Swelling and pain in the feet
- Stiffness in the feet
- Pain on the ball or sole of feet
- Joint shift and deformation
Diagnosis
Quick diagnosis of RA in the feet is important so that the podiatrist can treat the area effectively. Your doctor will ask you about your medical history, occupation, and lifestyle to determine the origin of the condition. Rheumatoid Factor tests help to determine if someone is affected by the disease.
If you have any questions please feel free to contact one of our offices located in St. Augustine, and Palatka, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Rheumatoid Arthritis in the Feet
Rheumatoid Arthritis is a chronic progressive disease that attacks several joints throughout the body. It is an autoimmune disease in which the body’s immune system mistakenly attacks the joints. As a result, the tissue inside the joints, called synovium, starts to thicken and causes pain around the joints. The synovium is responsible for creating a fluid that lubricates the joints to help them move. Approximately 1.5 million people in the United States have Rheumatoid Arthritis. Women are almost three times as likely to have RA compared to men, and it’s disease usually begins between the ages of 30 and 60. People who have a genetic history of RA are more likely to develop the disease.
Symptoms of RA may include the following sensations in the joints: pain, tenderness, swelling, redness, warmth, stiffness, and loss of range. Swollen joints are a very common symptom for those with the disease. At times, it may be minimal, but it may also be very apparent. Another typical symptom is joint stiffness. Doctors will often use the direction of morning stiffness to measure the severity of a patient’s joint inflammation. Other RA symptoms include limping, anemia, fever, and fatigue.
To diagnose RA, your podiatrist will typically request x-rays to see how much damage there is in the joints. Blood tests may also be performed to show if there are any signs of anemia, or antibodies such as the rheumatoid factor. If you have previously been diagnosed with RA, you should know the disease may spread to your feet and ankles.
There are many non-surgical options that can be used to treat this ailment. Some of these options include physical therapy, foot massages, orthotics, bracing, supportive shoes, and steroid injections. Physical therapy is useful because it will help stretch and strengthen the joints in both the foot and ankle to improve joint function. Massages can help improve blood circulation which will be good for the feet. Choosing proper footwear will allow you to walk with comfortability if you are a sufferer from RA. Lastly, bracing will help stabilize the foot joints, limit deformities and decrease pain.
In severe cases, surgery may be a treatment option that should be considered. For those who cannot walk without experiencing pain and those whose deformities can not be managed with braces, surgery should be considered. Your podiatrist will recommend surgery if he or she believes it will improve your foot biomechanics.
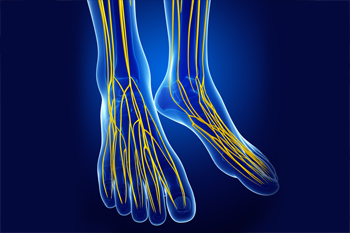
Tarsal Tunnel Syndrome Causes
The tarsal tunnel is a narrow space in the inner ankle that has nerves, blood vessels, and tendons passing through it. When the posterior tibial nerve inside of the tarsal tunnel is compressed, this leads to a painful condition called tarsal tunnel syndrome. Symptoms of this condition include foot pain, a pins and needles sensation, numbness, and swelling. The nerve compression that brings about tarsal tunnel syndrome can be caused by sports injuries, lesions, such as ganglion cysts, that occupy space in the tunnel, excess fluid buildup, changes in the biomechanics of the foot, wearing tight, ill-fitting shoes, or other medical conditions like diabetes and arthritis. In about 30% of cases, the cause is unknown. Nevertheless, tarsal tunnel syndrome can be treated and usually resolves within several weeks of treatment. If you have symptoms of this condition, please seek the care of a podiatrist.
Tarsal tunnel syndrome can be very uncomfortable to live with. If you are experiencing tarsal tunnel syndrome, contact one of our podiatrists of Coastal Foot & Ankle Wellness Center, LLC. Our doctors can provide the care you need to keep you pain-free and on your feet.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, which can also be called tibial nerve dysfunction, is an uncommon condition of misfiring peripheral nerves in the foot. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome, the tibial nerve is damaged, causing problems with movement and feeling in the foot of the affected leg.
Common Cause of Tarsal Tunnel Syndrome
- Involves pressure or an injury, direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or near the knee.
- Diseases that damage nerves, including diabetes, may cause tarsal tunnel syndrome.
- At times, tarsal tunnel syndrome can appear without an obvious cause in some cases.
The Effects of Tarsal Tunnel Syndrome
- Different sensations, an afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg.
- The foot muscles, toes and ankle become weaker, and curling your toes or flexing your foot can become difficult.
- If condition worsens, infections and ulcers may develop on the foot that is experiencing the syndrome.
A physical exam of the leg can help identify the presence of tarsal tunnel syndrome. Medical tests, such as a nerve biopsy, are also used to diagnose the condition. Patients may receive physical therapy and prescriptive medication. In extreme cases, some may require surgery.
If you have any questions please feel free to contact one of our offices located in St. Augustine, and Palatka, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Treating Tarsal Tunnel Syndrome
Tarsal tunnel syndrome is a condition in which the tibial nerve, located in the tarsal tunnel in the foot, is compressed. The tibial nerve can become compressed from injury, such as an ankle sprain, flat feet, and lesions. Arthritis, diabetes, and varicose veins can also cause swelling and thus result in nerve compression.
Symptoms of tarsal tunnel syndrome include several different sensations in the sole of the foot, inside the ankle, and around the tibial nerve. These sensations include shooting pains, numbness or reduced sensation, pins and needles, burning, and tingling. Symptoms tend to worsen with greater activity to the area. In rare and severe occasions, this can change the muscles in the foot.
If you suspect you have tarsal tunnel syndrome, you should consult with your podiatrist. He or she will examine your medical history to see if you have a history of diabetes, arthritis, or flat feet. They will also check to see if you have suffered an injury to the area recently. An electrical test will be conducted to check if the nerve has been damaged. A simpler Tinel’s Test might also be used. This includes simply tapping the nerve to create a sensation. An MRI scan of the area may also be used.
Treatments vary greatly for tarsal tunnel syndrome. Treatments include both nonsurgical and surgical options depending upon the severity of the condition. Nonsurgical options include anti-inflammatory medication and steroid injections to the area. Orthotics, such as a splint or brace that immobilizes the foot, is another noninvasive option. For those with flat feet, custom shoes can be made to offer better foot support. Surgical options include a tunnel tarsal release, in which an incision is made behind the ankle down to the arch of the foot. This releases the ligament and relieves pressure off the nerve. Some doctors use a more minimally invasive surgery, where smaller incisions are made in the ankle and the ligament is stretched out.
If you are suffering from painful sensations in your foot, see a podiatrist who can determine if you are experiencing tarsal tunnel syndrome. Tarsal tunnel syndrome that is left unchecked can cause permanent nerve damage to the foot.
Why Live with Pain and Numbness in Your Feet?
Obesity and the Feet in Older Adults
Obesity affects every part of your body - including your feet and ankles. People over 60 who are obese have been found to experience more foot pain, have reduced toe and ankle strength, and have a slower walking speed, among other problems. Excess body weight strains the lower limbs, leading to functional and structural changes that can impact your mobility and quality of life. This is particularly the case for older adults. One of the best ways to maintain the health of your feet and improve your overall health is to eat a healthy diet, exercise, and lose weight. Unfortunately, this can be very difficult if you have foot and ankle pain that makes it harder to exercise or even stand for long periods of time. A podiatrist can help you reduce foot and ankle pain and increase your mobility so that you can improve your quality of life. For more information, please consult with a podiatrist.
The more you weigh, the harder your feet must work to support your body. If you’re an obese individual and are concerned about your feet, contact one of our podiatrists from Coastal Foot & Ankle Wellness Center, LLC. Our doctors can provide the care you need to keep you pain-free and on your feet.
Obesity and Your Feet
People who are overweight are putting more pressure on their ankles, knees, and hips as well as their feet. This unfortunately can lead to variety of different issues.
Problems & Complications Stemming from Obesity
- When the body is overweight, it tries to compensate by changing the way that it moves. An obese person may lean forward and put extra weight on the wrong part of the foot. This puts unnecessary stress on the feet.
- Obese people are also more likely to develop type II diabetes which is a condition that causes a lot of foot problems. People with diabetes often don’t feel the cuts and sores that they may have on their feet, which can lead to more complicated and severe issues.
- Plantar fasciitis is another foot condition that can be caused by obesity. Plantar fasciitis is an inflammation of the tissue along the bottom of the foot, which causes pain and stiffness while walking and climbing stairs.
If you have any questions, please feel free to contact one of our offices located in St. Augustine, and Palatka, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.